Cat bites, often underestimated due to their seemingly minor appearance, are a significant cause of infection. While dog bites are more frequent, cat bites are responsible for a higher percentage of bite-related infections. This article delves into the dangers of Infected Cat Bites, how to recognize them, and the necessary treatments, drawing from a compelling case study.
The Underestimated Threat of Cat Bites
It’s easy to dismiss a cat bite as a mere scratch, but the anatomy of a cat’s mouth makes these injuries particularly prone to infection. Cats possess sharp, needle-like teeth that can penetrate deeply into tissues, joints, and even bone. These puncture wounds, often less visually dramatic than dog bites, inject bacteria-laden saliva deep beneath the skin. This creates an ideal environment for infection to thrive, hidden from easy cleaning and the body’s natural defenses. The resulting “dead space” under the skin allows bacteria to multiply, leading to potentially serious complications if left untreated.
Identifying an Infected Cat Bite: Symptoms to Watch For
Infection from a cat bite typically manifests rapidly. Within 24 hours, approximately 70% of individuals will experience noticeable signs of infection, increasing to 90% within 48 hours. Key symptoms to watch for include:
- Intense Pain: Beyond the initial bite, pain will escalate and become throbbing.
- Redness (Erythema): The area around the bite will become increasingly red and inflamed.
- Swelling (Edema): Swelling will develop around the wound site.
- Warmth: The skin around the bite may feel warm to the touch.
- Pus or Drainage: Discharge from the wound is a clear sign of infection.
- Fever: A rise in body temperature indicates a systemic response to infection.
- Lymphangitis: Red streaks extending from the wound towards the elbow or groin, indicating infection spreading through the lymphatic system.
 Hand with infected cat bite wounds showing redness and swelling
Hand with infected cat bite wounds showing redness and swelling
Image: Close-up of a hand displaying multiple puncture wounds from an infected cat bite, characterized by significant erythema and edema around the wrist and thenar muscle, with lymphangitis extending up the arm.
Certain factors increase the risk of severe infection after a cat bite. These include:
- Diabetes Mellitus: Compromised immune response.
- Immunocompromised Conditions: Weakened immune system.
- Older Age: Slower healing and potentially weaker immune response.
- Delayed Treatment: Allowing infection to progress.
- Inadequate Initial Care: Improper wound cleaning.
In severe cases, untreated infected cat bites can lead to serious complications like sepsis, multi-organ failure, and even death.
Case Study: A Rapidly Developing Cat Bite Infection
Consider the case of a 60-year-old woman who sought emergency care after being bitten by her cat. Just one day after the incident, she presented with a fever of 38.5°C (101.3°F), general malaise, and three deep puncture wounds on her right hand and wrist. The wounds were visibly red, swollen, and intensely painful (rated 8/10 on a pain scale). Alarmingly, red streaks indicated lymphangitis spreading up her arm.
Blood tests revealed elevated white blood cell counts (15.8×10^9/L, normal range: 4.0-10.0×10^9/L) and a significantly elevated C-reactive protein level (224.9 mg/L, normal: <2), both strong indicators of infection.
Prompt surgical intervention was necessary. The wounds were surgically debrided, irrigated, and drained. Empirical antibiotic therapy with oral amoxicillin/clavulanic acid was initiated. This combination antibiotic is effective against a broad spectrum of bacteria commonly found in animal bites.
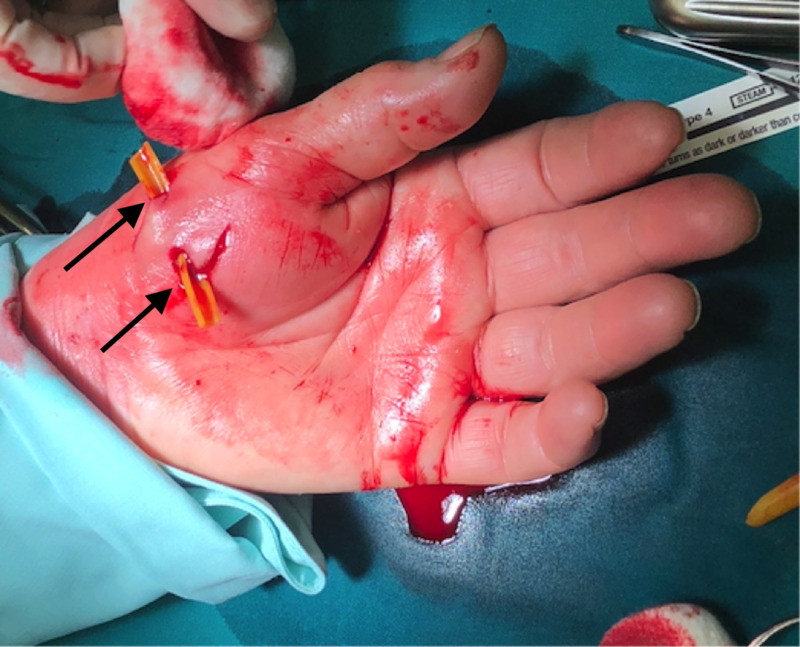 Surgical debridement and irrigation of infected cat bite wounds
Surgical debridement and irrigation of infected cat bite wounds
Image: Surgical site showing debridement and irrigation of infected cat bite wounds on a hand, with a catheter placed for drainage.
While wound cultures were sterile, serological tests confirmed the presence of Bartonella henselae, the bacteria responsible for cat scratch disease. This highlights that even when standard bacterial cultures are negative, specific pathogens like Bartonella can be involved in infected cat bites.
The patient responded well to treatment. Her inflammatory markers decreased, and she was discharged after a few days, with complete resolution of the infection and no lasting hand function impairment.
Common Bacteria in Infected Cat Bites
A variety of bacteria can be introduced into a cat bite wound. The most common culprits include:
- Pasteurella species: Frequently found in the mouths of cats and dogs, and the most common bacteria isolated from bite wounds.
- Streptococci and Staphylococci: Common skin bacteria that can also cause wound infections.
- Neisseria and Moraxella species: Other bacteria found in the oral flora of cats.
- Bartonella henselae: The cause of cat scratch disease, transmitted through scratches or bites.
Cats can carry Bartonella henselae without showing symptoms themselves. Transmission to cats often occurs through flea bites. While Bartonella henselae is well-known for causing cat scratch disease from scratches, it’s important to recognize it can also be transmitted through bites, as illustrated in the case study. In cases where Bartonella henselae serology is negative, another species, Bartonella clarridgeiae, should be considered.
Treatment Strategies for Infected Cat Bites
Prompt and appropriate treatment is crucial for managing infected cat bites and preventing serious complications. Treatment typically involves:
- Wound Cleaning and Debridement: Thoroughly cleaning the wound with soap and water is the first step. Deeper puncture wounds may require surgical debridement to remove dead tissue and bacteria, as seen in the case study.
- Irrigation and Drainage: Flushing the wound with sterile saline solution helps to remove bacteria and debris. Deep wounds may require drainage to prevent abscess formation.
- Antibiotic Therapy: Antibiotics are essential to combat bacterial infection. Amoxicillin/clavulanate is often the first-line treatment. For individuals with penicillin allergies, alternatives include fluoroquinolones or trimethoprim/sulfamethoxazole. Doxycycline can be used for patients over 10 years old.
- Tetanus Prophylaxis: A tetanus booster may be necessary depending on the patient’s vaccination history.
- Pain Management: Pain relief medication may be needed to manage discomfort.
While X-rays are sometimes used to check for retained teeth fragments, they are not very specific for detecting infection. MRI might be used in some cases, but surgical exploration and debridement often provide the most direct assessment and treatment.
Prevention is Key
While not all cat bites can be prevented, taking precautions can significantly reduce the risk:
- Understand Cat Behavior: Learn to recognize signs of feline aggression or fear to avoid provoking a bite.
- Gentle Interaction: Handle cats gently and avoid sudden movements that might startle them.
- Avoid Provocation: Do not tease or play roughly with cats, especially stray or unfamiliar animals.
- Vaccination and Flea Control: Keeping cats vaccinated and on flea control can reduce the risk of carrying and transmitting certain infections.
- Seek Medical Advice: If bitten by a cat, even if the wound seems minor, clean it thoroughly and consult a doctor, especially if signs of infection develop.
Conclusion: Taking Cat Bites Seriously
Infected cat bites are a significant health concern that should not be underestimated. Their puncture wound nature and the bacteria present in a cat’s mouth create a high risk of infection. Prompt recognition of infection symptoms and immediate medical intervention, including surgical debridement and antibiotic therapy, are crucial for successful treatment and preventing serious complications. By understanding the risks and taking preventive measures, individuals can minimize the likelihood of experiencing an infected cat bite and ensure prompt care if one occurs.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare professional for diagnosis and treatment of any medical condition.
